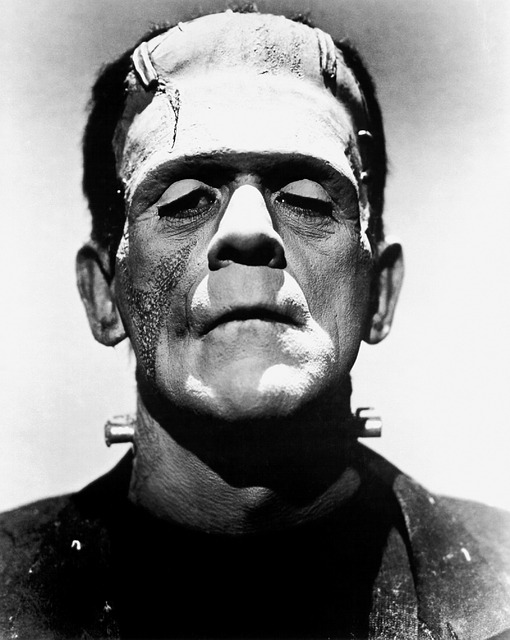
Herniated Discs – Natural Spinal Care Vs Standard Medical Frankenstein Treatments
Spinal disc herniation (often called a ‘herniated’ or ‘slipped’ disc) is a relatively common cause of back problems, and can cause severe pain and disability. Herniated discs are caused when a tear in the outer, fibrous ring of a spinal disc causes the soft, central portion to protrude out, usually as a result of taking poor care of oneself. Contrary to popular belief it has very little to do with ageing, improper lifting or trauma – and if you hear someone telling you this you should be aware that you’re dealing with someone who is unaware of the latest research. When the back pain radiates out and nerves are compressed the resulting pain can be particularly excruciating and persistent; however, minor problems are more common. As with all pain, herniated discs can cause acute pain, or develop into chronic pain lasting over a few months.
Standard “Frankenstein” Treatments for Herniated Discs
Weight bearing magnetic resonance imaging (MRI) provides the most conclusive method of diagnosing herniated discs, by producing 3-D images of the spinal cord, nerve roots, and surrounding areas.Unfortunately, virtually all MRIs taken to diagnose disc herniations in the US are taken lying down and these are diagnostically useless in most cases since the disc is not under strain.
Another very accurate method for diagnosing herniated discs is weight bearing digital x-ray with Posture Ray analysis, which is what we use at Rittenhouse Square Chiropractic. This method is so accurate that there are virtually no advantages with weight bearing MRI, and its light years ahead of supine MRIs…Minor disc problems are usually treated with non-steroidal anti-inflammatory drugs (NSAIDS), which are generally quite effective in managing the pain. However, there are serious question marks over the side effects of medium or long-term NSAID use, which we look at below.
Alternatively, epidural steroid injections may be employed in more serious cases. These are injections of cortisone directly into the spine near to the location of the pain. Again these have good results in the short-term management of the pain itself, but there are concerns over their side effects.
Finally, in the most severe cases, disc problems may be treated with surgical intervention. A technique called lumbar fusion may be used for recurrent herniations, whereby two or more vertebrae are surgically joined together using bone tissue from the patient or a donor. In combination with the body’s natural bone growth processes the vertebrae become fused together over the course of time. This is a process not without complications, as we shall see below.
Several other surgical options include the following:
- Chemonucleolysis – where the protruding disc is dissolved.
- Tessys method – which removes herniated discs using an endoscopic method.
- Laminectomy – which relieves spinal stenosis or nerve compression.
- Artificial disc replacement.
Impulse Incision Technique for Disc Pain
In the standard medical community, where great stock is placed in medicating and surgical intervention, natural spinal care has often received short shrift. Much of the standard medical literature would have patients believe that there is a lack of evidence available to demonstrate that natural spinal care works. However, the studies have been done and are available, but rarely make the light of day in the mainstream.
There is plenty of quality recent evidence that natural spinal care is effective for the treatment of acute and chronic lumbar disc herniation and its associated pain, and that it carries fewer risks than other traditional treatment methods outlined above. We start by looking at the evidence of how natural spinal care compares with some of these other treatment methods.
Comparative Effectiveness: Natural Spinal Care and Lumbar Nerve Root Injections
A study published last year in the Journal of Manipulative and Physiological Therapeutics looks at the results of patients with lumbar disc herniations treated with high-velocity, low-amplitude spinal thrusts (Impulse Incisions) compared with those receiving imaging-guided lumbar nerve root injections (NRI). This was a prospective cohort comparative effectiveness study based on self-reported pain in over 100 age- and sex-matched patients.
Results showed that over three-quarters of patients treated with Impulse Incisions reported improvement in their pain; whilst just under two-thirds of patients treated with NRI reported easing of their pain. Both methods could be claimed to be effective for pain treatment, though the average cost of Impulse Incision Technique was slightly less than that for NRI; so it is tempting to lean towards the natural method as the better option, even before we begin to consider potential side effects.
An even more recent study, involving members of the same team and published this year in the same journal, examined the longer-term effects of Impulse Incisions by following up over a period of one year after the original study. In this way the authors were able to determine whether Impulse Incisions has the same positive effect on chronic pain as it does on acute pain.
The same high-velocity, low-amplitude, spinal procedure was used on almost 150 patients with LBP and leg pain, due to lumbar disc herniations. The results showed ‘significant improvement’ for all outcomes at all time points for a large percentage of patients: ‘At 3 months, 90.5% of patients were “improved” with 88.0% “improved” at 1 year. Although acute patients improved faster by 3months, 81.8% of chronic patients reported “improvement” with 89.2% “improved” at 1 year. There were no adverse events reported.’
Note the final sentence above, as this is key: ‘There were no adverse events reported.’ The same cannot be said for some of the standard recommended treatments for disc herniation, as we see below.
Side Effects of Epidural Injections
A US study from 2013, published in The Journal of Bone and Joint Surgery, analyzed patients with vertebral body fractures following epidural steroid injections. Lumbar epidural steroid injections (LESIs) are often prescribed for the treatment of pain arising from compression of the spinal nerves. The study set out to examine whether fears about corticosteroids adversely affecting bone strength and therefore increasing the risk of vertebral bone fracture, were well-founded.
From over 50,000 patients with serious spinal disease, over 3000 of those who had received at least one LESI were included in the study. Also included were 3000 others who had received no injection and were well matched with factors like age, sex, race, hyperthyroidism, and steroid use.
Here are the findings, in summary:
‘In the survival analysis, an increasing number of injections was associated with an increasing likelihood of fractures. Each successive injection increased the risk of fracture by a factor of 1.21.’ – That’s 21% people!!!
It is therefore hard to escape the conclusion that LESIs, one of the most common forms of treatment for serious back pain, is fundamentally flawed because it leads to increased bone fragility and the problems that accompany that (notably increased fracture risk).
Advice from the study authors is that ‘LESIs should be approached cautiously in patients at risk for osteoporotic fractures.’
Side Effects of NSAIDS
In the light of concerns expressed over the cardiovascular safety of NSAID use, a 2010 Danish study published in Circulation, the journal of The American Heart Foundation, examined the potential cardiovascular side effects associated with usage of these drugs.
The study included over a million of the 2.63 million plus Danes (57.8% of the population) who had claimed at least 1 prescription for NSAIDs between 1997 and 2005. Individuals without hospitalizations 5 years before their first prescription claim of NSAIDs were selected for the study. It was found that, although not all NSAIDs had the same effects, some of the most commonly-prescribed drugs were associated with increased cardiovascular mortality and morbidity:
“Use of the nonselective NSAID diclofenac and the selective cyclooxygenase-2 inhibitor rofecoxib was associated with an increased risk of cardiovascular death, with a dose-dependent increase in risk.”
‘There was a trend for increased risk of fatal or nonfatal stroke associated with ibuprofen treatment.”
The study authors unsurprisingly conclude that many NSAIDs should be “used with caution in most individuals”.
Side Effects of Lumbar Fusion Surgery
In a historical cohort study conducted to find out about the long-term effects of lumbar fusion, the objective was to determine the outcomes of return to work (RTW), permanent disability, post-surgical complications, opiate utilization, and re-operation status for chronic low back pain sufferers who had had the surgery. The study examined 725 lumbar fusion cases compared to the same number of controls, randomly selected from subjects with chronic low back pain diagnoses.
Below is a summary of the key results:
- Two years after fusion surgery, 26% of fusion cases had RTW, while 67% of nonsurgical controls had RTW, within 2 years from the date of injury.
- The re-operation rate was 27% for surgical patients.
- Of the lumbar fusion subjects, 36% had complications.
- Permanent disability rates were 11% for cases and 2% for non-operative controls.
- 17 surgical patients and 11 controls died by the end of the study.
- For lumbar fusion subjects, daily opioid use increased 41% after surgery.
The following was the sobering conclusion from the study authors, based on these results:
“Lumbar fusion for the diagnoses of disc degeneration, disc herniation, and/or radiculopathy ….is associated with significant increase in disability, opiate use, prolonged work loss, and poor RTW status.”
The Bottom Line
The clear conclusion, from even a cursory scan of the available studies, must be that there is more to spinal disc herniation treatments than doctors are passing on to patients. The fact is that success rates with natural spinal care hold up well against some of the common treatments and are better than others. In other words, they relieve pain just as well or better. BUT they work without the frequent risk of severe side effects or adverse events, and often without the costs involved in these treatments.
Natural spinal care is one of the safest if not the safest treatment for back pain and herniated discs, and beyond that natural spinal care doesn’t just relieve the pain a herniated disc might be causing, this approach also re-builds the disc restoring it to robust health again, something drugs, injections and surgery can NEVER claim!
If you have back pain and are considering an epidural to relieve your pain consult with the chiropractors at Rittenhouse Square Chiropractic. Call (215) 546-1010 for an appointment or click here to book online.